How to deal with monitor glare
To get rid of glare and thus reduce strain, first of all, you should place the computer monitor so that the windows are located to the side. If this is not possible, then you should close the curtains so that excess light does not fall on the screen. Bright ceiling lights should be turned off or replaced with lamps of lower intensity. The desk light should be positioned so that it does not shine directly on the screen and into the eyes.
In addition, the use of computer glasses with special anti-glare coating gives good results.
The brightness of the computer screen should be adjusted - it should not be too bright, but not dim.
The eye perceives information more easily if high contrast is set in the monitor settings. The color of the screen is also important - it is desirable to work on a black and white or light yellowish background.
The brightness of the general lighting in the room should match the brightness of the monitor. All this reduces the likelihood of developing computer vision syndrome.
It is recommended to take short breaks from work, every 10-15 minutes. During this time, you can focus your eyes on objects outside the window or in the distance if there is no window nearby. The eyes should be given a rest at least once an hour. It is advisable to perform exercises that relieve eye fatigue.
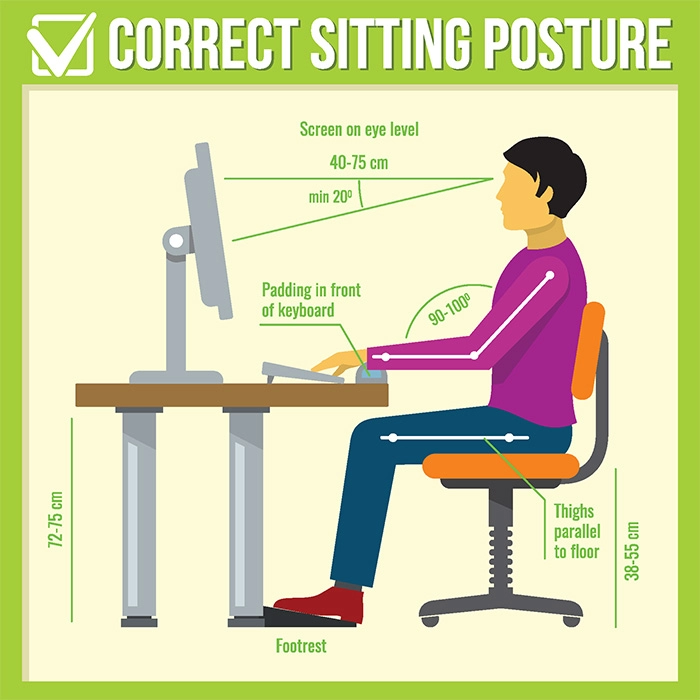
Why is it important to sit correctly
The visual image is formed in the occipital lobe of the brain. The full blood supply of these sections depends on the health of the vessels of the cervical region. Incorrect position of the body, head and neck contribute to muscle spasm and tension, which in turn leads to compression of the carotid and vertebral arteries and a decrease in oxygen supply. This condition leads to weakness and dizziness, fatigue. Physiotherapy measures reduce the risk of developing complications and prevent the occurrence of computer vision syndrome.
Prevention is always preferable to treatment, so you should properly organize the workspace and computer monitor so that the eyes do not suffer. It is recommended to use moisturizing drops, eat foods rich in vitamins.
Any eye diseases, including computer vision syndrome, require consultation with
a highly qualified specialist who will select the safest and most effective treatment tactics.