Complete blood count
26 February 2026
A Complete blood count (CBC) is one of the most valuable and widely used blood tests in healthcare. With a small sample of blood, it provides a broad overview of how your body is functioning. Doctors rely on it not only to detect diseases, but also to monitor overall health, evaluate treatments, and identify early warning signs before symptoms become severe.
Blood is more than just a red liquid — it is a living tissue made up of different types of cells, each with a specific purpose. A CBC measures the number, size, and characteristics of these cells, helping healthcare providers understand what may be happening inside your body.
What does a CBC measure?
A Complete Blood Count focuses on three essential components:
• Red blood cells (RBCs) – These cells transport oxygen from your lungs to all tissues and organs. The test also measures hemoglobin (the oxygen-carrying protein) and hematocrit (the percentage of blood made up of red cells). Abnormal levels may suggest anemia, dehydration, or other medical conditions.
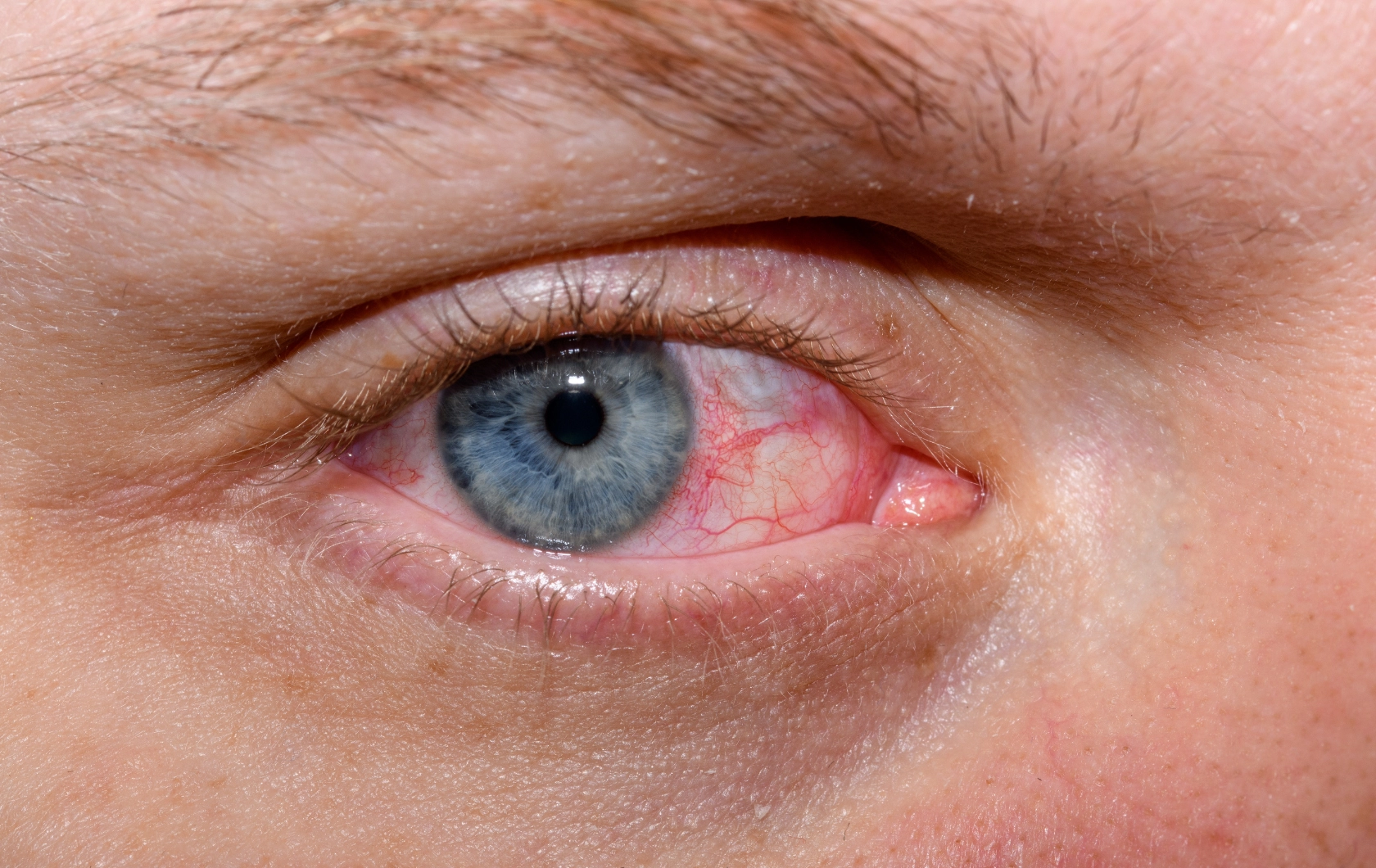
• White blood cells (WBCs) – These are the body’s defense cells. They fight infections and respond to inflammation. When necessary, a CBC with differential gives a more detailed breakdown of the different white blood cell types, offering clues about infections or immune system activity.
• Platelets – Platelets help your blood clot properly. Too few platelets may increase bleeding risk, while too many may increase the risk of unwanted clotting.
Together, these measurements create a detailed snapshot of your internal balance.
When and why is it ordered?
A CBC is commonly included in routine health checkups, even if you feel completely well. However, doctors may also order it to:
• Investigate symptoms such as fatigue, fever, weakness, bruising, or unexplained weight loss
• Monitor chronic conditions like kidney disease, immune disorders, or cancer
• Evaluate how medications or treatments are affecting blood cell production
Because blood cells respond quickly to stress, infection, and inflammation, the CBC often serves as an early indicator of change within the body.
How the test is performed
The procedure is simple and usually takes only a few minutes. A healthcare professional draws blood from a vein in your arm using a small needle. The sample is sent to a laboratory, where automated equipment counts the cells and analyzes their size and structure. If needed, a specialist may review the sample under a microscope for additional detail.
Most people do not need special preparation before a CBC. You can typically eat and drink normally unless other blood tests are being done at the same time.
Understanding the results
It is important to remember that abnormal numbers do not automatically mean a serious illness. Factors such as hydration, stress, nutrition, medications, or minor infections can temporarily affect blood counts. For this reason, doctors interpret results in the context of your symptoms, medical history, and sometimes additional tests.
Despite its simplicity, the complete blood count remains one of the cornerstones of modern medicine. It offers a powerful glimpse into your body’s health — quietly revealing whether everything is functioning in harmony or signaling that further attention may be needed.