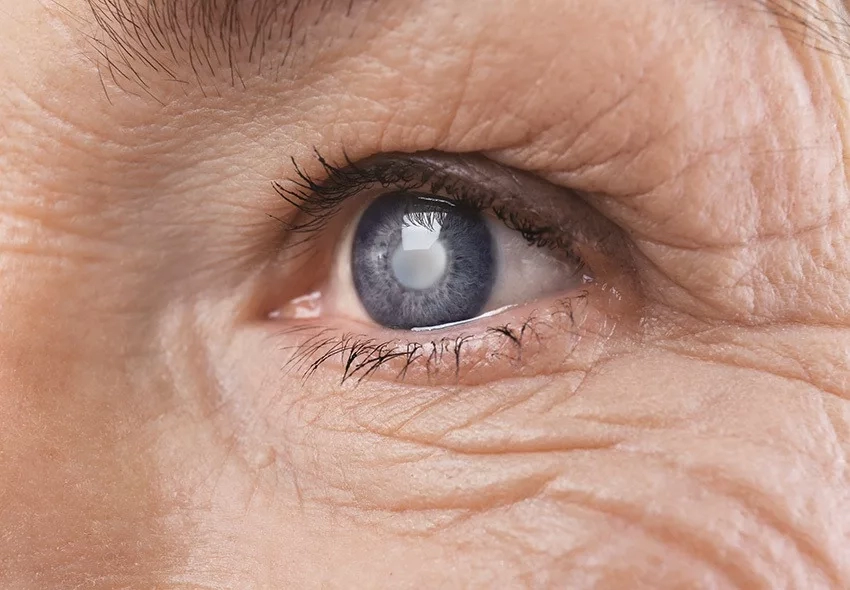
During the international congresses, ophthalmological conferences and symposia organized by the Association of Cataract and Refractive Surgeons of Armenia, the most modern methods of cataract surgery, avoiding complications, new, more effective approaches are constantly discussed and discussed.
Cataract surgery is performed under local anesthesia, is painless, without stitches, lasts 20-30 minutes, and the patient does not need to be hospitalized. It is also possible to place multifocal lenses in the eye socket, if the patient wishes, which correct age-related vision/presbyopia/, thus relieving the patient of the need to wear glasses for near vision. The recovery period is 2-3 weeks, during which mainly application of topical drops; Immediately after the operation, the haze disappears, vision becomes clear and may improve even more over the next 2-3 weeks. During this period, it is recommended to refrain from
sudden movements, sports, saunas, swimming pools, and physical exertion.
After 1 month, you can return to normal life.
This modern ultrasound cataract surgery significantly improves vision, is less traumatic, less stressful, and helps to dramatically improve the patient's quality of life.
Now the most important question is when is the most favorable and appropriate time for the operation.
The point is that this ultrasound method is applicable in the presence of subtle clouding of the lens, but not in the case of hardened, old cataracts. Therefore, in order to make the right choice, an
ophthalmologist's consultation is necessary in order to ensure a favorable outcome of the operation and avoid postoperative complications.